The key to great population health management is the ability to integrate quality programs that deliver better health outcomes.
Integrated Approach
The majority of TPA services outsource their medical management and therefore minimize the interaction between employees and nurse. Through our integration with HealthCheck360, SISCO takes a more active approach to medical management with a service model that benefits all.
SISCO's Model
![]()
Member Communication
Encourage member communication with the Doctors & Nurses of HealthCheck360.
![]()
Medical Management
Integrate TPA & Medical Management technology to enhance Nurse intervention, timing, and results complex cases.
Case Management
The Case Management program is a collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates options and services for complex cases.

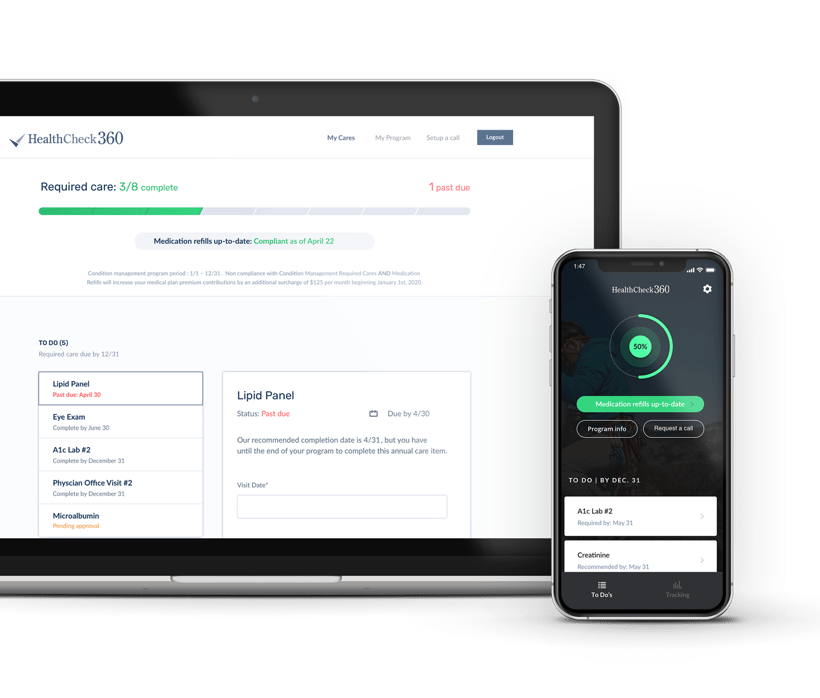
Condition Management
Condition Management helps members with complex health conditions improve outcomes through a combination of education and treatment strategies. Our team of medical professionals are committed to helping members make positive change to improve health, while increasing productivity and reducing costs. It includes:
Utilization Management
Utilization Management ensures the delivery of medically necessary services and improves access to quality care. Outreach from a dedicated Registered Nurse means that evidence-based, clinical guidelines are applied to each request.

![]()
My nurse was truly a godsend. She helped me through my entire cancer experience. I truly thank her for her support.
—
PARTICIPANT